A few weeks ago I was chatting to an expecting mum and during this conversation she had told me that her obstetrician had told her in regard to third stage (placenta deliver) she would need a shot, to help birth the placenta and stop the bleeding. She was told everyone has it, she would have little choice – it was what was done and when she asked about it, the options given to her as a reason why it was done – where for pure convenience.
She went home and researched and asked her friends and what she found was that it was something most women had done, that it was common practice! I wanted to hold her hand as she went to discuss things with her obstetrician, I wanted to be there and support her when she told them “NO”.
The medical management of the third stage of labour- the time between the baby’s birth, and the emergence of the placenta it very common. We have injections, examinations, and clamping and pulling on the cord. Instead of skin-to-skin contact, bonding and body heat, we have separation, inspections and wrapping, and then we have haste to deliver the placenta and clean up for the next ‘case’.
As Sarah Buckley of Gentle Birth, Gentle Mothering has also written “Medical management of the third stage, which has been taken even further in the last decade, with the popularity of ‘active management of the third stage’ which has its own risks for mother and baby. While much of the activity is designed to reduce the risk of maternal bleeding, or postpartum haemorrhage (PPH), which can be a serious event, it seems that, as with the active management of labour, the medical approach to labour and birth may actually lead to many of the problems that active management is designed to address.”
The use of active management also creates specific problems for mother and baby. In particular, the use of active management leads to a newborn baby being deprived of up to half of his or her expected blood volume. This extra blood, which is intended to help the newly functioning lungs and other vital organs, is discarded along with the placenta when active management is used.
Synthetic oxytocin has also been linked to an increased risk of postpartum depression. In a recent study, it was found that women with a history of depression or anxiety disorder prior to pregnancy, exposure to peripartum oxytocin increased the risk of postpartum depression or anxiety disorder by 36%. Women with no history of prepregnancy depressive or anxiety disorder, exposure to peripartum oxytocin increased the risk of postpartum depressive or anxiety disorder by 32% compared to those not exposed.
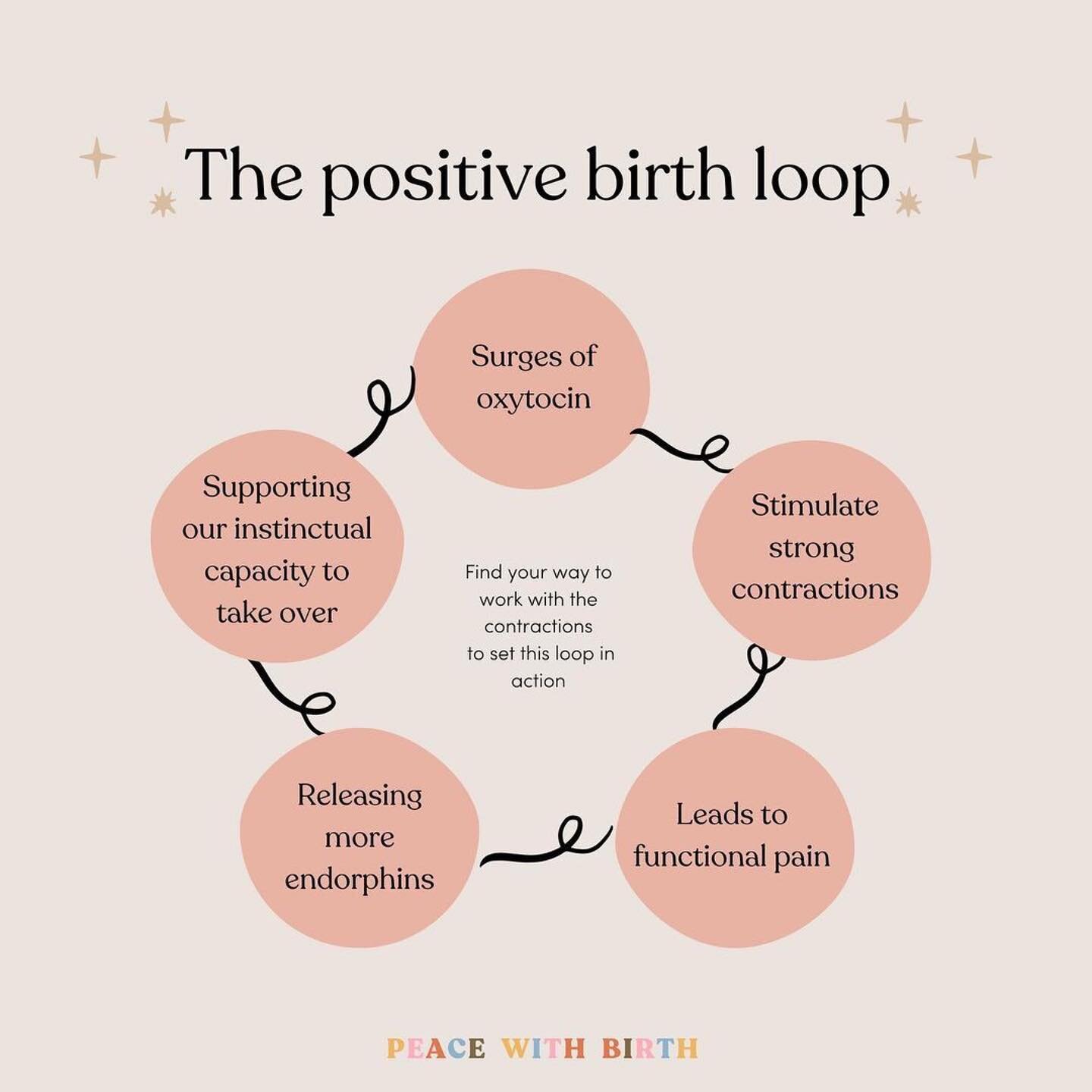
Sarah also speaks of the hormones that occur during the third stage of labour, so when we inject a synthetic into the workings of our natural hormones those connections change and ultimately will affect mother and baby. What naturally occurs during the third stage of labour is strong uterine contractions continue at regular intervals, under the continuing influence of oxytocin. The uterine muscle fibres shorten, or retract, with each contraction, leading to a gradual decrease in the size of the uterus, which helps the placenta pull away from its attachment site on the mother’s uterine wall. Third stage is complete when the mother delivers her baby’s placenta.
During this time the Mothers has peak levels of oxytocin, the hormone of love, and endorphins, hormones of pleasure for both mother and baby. Skin-to-skin contact and the baby’s first attempts to breast-feed further augment maternal oxytocin levels, strengthening the uterine contractions that will help the placenta to separate, and the uterus to contract down. In this way, oxytocin acts to prevent haemorrhage, as well as to establish, in concert with the other hormones, the close bond that will ensure a mother’s care and protection, and thus her baby’s survival. (Buckley, 2005)
So why is this being ignored, knowing what we know about delayed cord clamping and the effects synthetic oxytocin can have on a mother postpartum, why are we not giving women a choice and a say in having a managed third stage and when do we say enough!
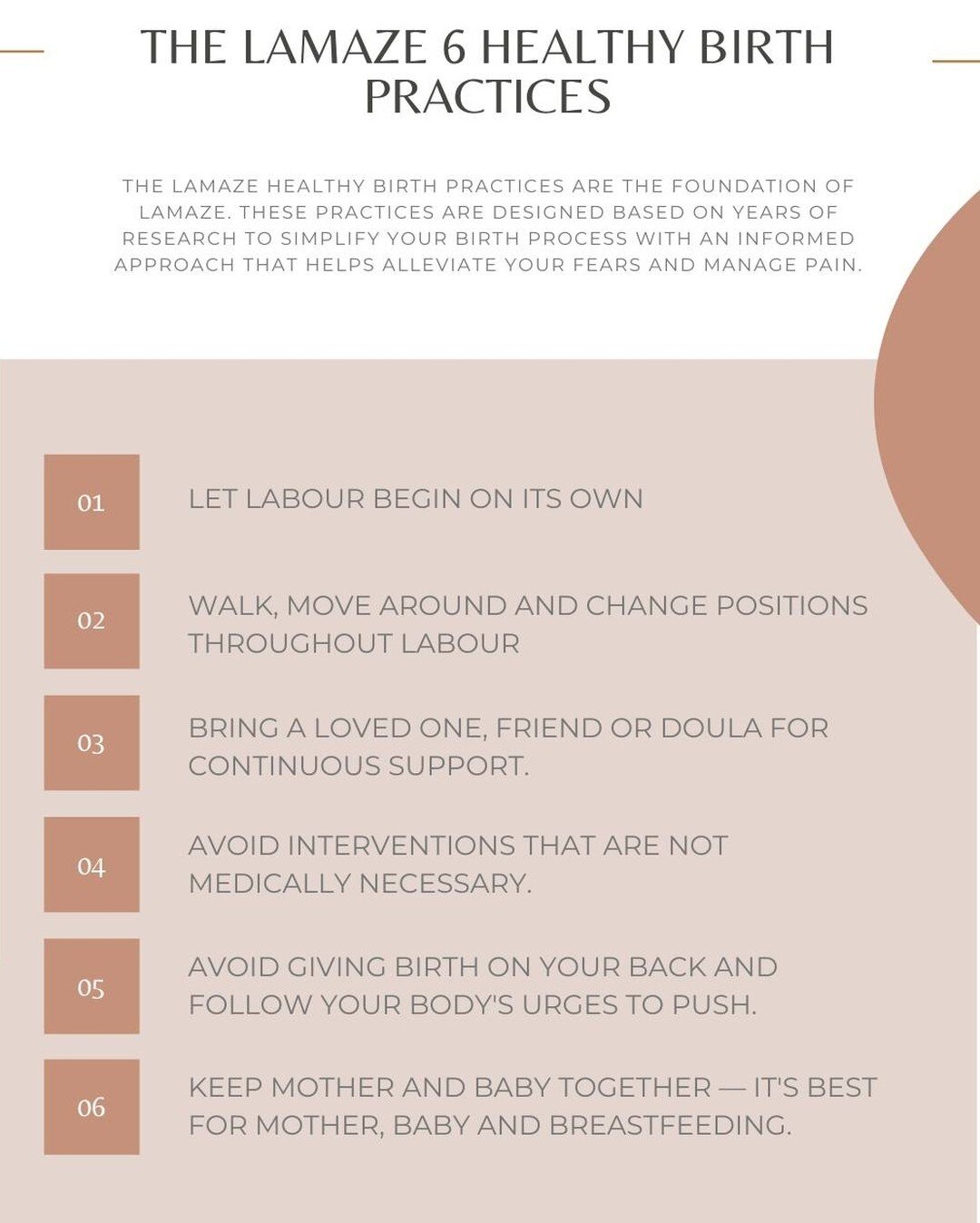
For me this is where childbirth education becomes highly important, where knowing the pros and cons of a managed third stage labour are taught, where being informed and being able to communicate with your care provider are vital – these are only just a few of the things expecting parents are taught in a Lamaze class.
Care professionals need to think about the birthing woman. Whilst most things are simply “routine” for them, they are not for a first time mother and full information and consent need to be given. Instead, most care professionals seem convinced that they know best, that mother’s do not know how to give birth and that birth is a medical emergency – when most births are not! They skim over information or just expect the mother to be a mind reader or get frustrated when she will not comply, when she will not do what they have told her.
All over the world, women are repeatedly forced to undergo procedures and interventions during labour and birth that they would not necessarily agree to. Had they been given all of the information and been able to make an informed decision, their choice would have been ‘no’. The decisions you make about your birth options can ultimately have long lasting effects on the health and wellbeing of yourself, your baby and your family.
Women who feel satisfied and in control of their birth experience are less likely to experience traumatic stress after birth. Ideally, women should be valued as the key decision maker in their own care by all caregivers.
In Birth, Gem.
References
Buckley, S., 2005. Leaving Well Alone: A Natural Approach to the Third Stage of labour. [Online]
Available at: http://sarahbuckley.com/leaving-well-alone-a-natural-approach-to-the-third-stage-of-labour
Kroll-Desrosiers A, N. B. B. J. G.-W. Y. M. S. T. D. K., 2017. Wiley Periodicals - Association of peripartum synthetic oxytocin administration and depressive and anxiety disorders within the first postpartum year.. [Online]
Available at: https://www.ncbi.nlm.nih.gov/pubmed/28133901
Rabe H, D. J. D. L. D. T., 2012. Effect of timing of umbilical cord clamping and other strategies to influence placental transfusion at preterm birth on maternal and infant outcomes.- Cochrane Database of Systematic Reviews. [Online]
Available at: http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD003248.pub3/abstract;jsessionid=3EE451A363B32133121955277B02EA9F.f02t01
Ruta Nonacs, M. P., 2017. Synthetic Oxytocin and Its Effect on Postpartum Mood and Anxiety - Womens Mental Health. [Online]
Available at: https://womensmentalhealth.org/posts/synthetic-oxytocin-effect-postpartum-mood-anxiety/